- LCGC-11-01-2020
- Volume 38
- Issue 11
Validation of Stability-Indicating HPLC Methods for Pharmaceuticals: Overview, Methodologies, and Case Studies

In the pharmaceutical industry, method validation is essential. But what are the best practices? We review regulatory requirements, validation parameters, methodologies, acceptance criteria, trends, and software tools.
This installment is the third in a series of three articles on stability testing of small-molecule pharmaceuticals. This article provides a comprehensive and updated overview of the validation of stability-indicating methods for drug substances and drug products, and addresses regulatory requirements, validation parameters, methodologies, acceptance criteria, trends, and software tools. Examples of generic protocols, reporting templates, and data summaries are included as supplemental reference resources.
The validation of analytical procedures used in regulated stability testing of drug substances (DS) and drug products (DP) is required by law and regulatory guidelines. For instance:
"The accuracy, sensitivity, specificity, and reproducibility of test methods employed by the firm shall be established and documented. Such validation and documentation may be accomplished in accordance with 211.194(a)" (1).
"The objective of validation of an analytical procedure is to demonstrate that it is suitable for its intended purpose" (2).
Method validation is the process of ensuring that a test procedure is accurate, reproducible, and sensitive within the specified analysis range for the intended application. Although regulatory authorities require method validation for the analytical procedures used in the quality assessments of DS and DP, the actual implementation is open to interpretation and may differ widely among organizations and in different phases of drug development. The reader is referred to regulations (1), guidelines (2–5), books (6–9), journal references (10, 11), and other resources (12) for further descriptions or discussions of associated regulations, methodologies, and common practices. This article focuses on methodologies for small-molecule DS and DP (such as tablets and capsules). Analytical procedures for biologics, gene and cell therapies, and genotoxic impurities are not discussed (6).
The purpose of method validation is to confirm that a method can execute reliably and reproducibly as well as ensure accurate data are generated to monitor the quality of DS and DP. It is essential to understand the intended use of the method to design an appropriate validation plan. The requirements of the plan also must be suitable for the phase of development, because method validation is an ongoing process through the life cycle of the product.
The method validation process can be broken down into three main steps: method design, method validation, and method maintenance (continued verification). Thus, the method itself continues to evolve throughout the product development life cycle. A method is typically “fully” validated at a late phase prior to testing of the biobatches (validation batches). Based on the International Council for Harmonization (ICH) Q6 guideline (13), analytical procedures are also part of the specifications that are submitted to and approved by a regulatory agency. Therefore, changes in a method must be monitored closely (13). After product launch, changes may need to be managed through a formal change control program, depending upon the changes, because prior approval from the regulatory agency, based on ICH Q10, may be required (14).
This section describes data elements required for method validation (see Figure 1) extracted from ICH Q2 (R1) and United States Pharmacopeia (USP) general chapter <1225> (3). Table I lists definitions of the required method validation parameters, extracted from ICH Q2 R1. Discussions of each parameter follow in the next section.
Table II lists the data requirements of different types of analytical procedures. as listed in USP <1225> (3). As described in the previous article in this series (15), the analytical procedures used today are predominantly “composite” reversed-phase liquid chromatography (RPLC) gradient methods with UV detection for the simultaneous determinations of both potency (active pharmaceutical ingredient, or API) and impurities and degradation products. These high-performance liquid chromatography (HPLC) methods often do double duty as a secondary identification test to supplement the spectroscopic identification (such as infrared or UV) of the API in DS or DP samples. For these reasons, the validation data elements required include those for USP Assay Category I (assay), Category II (quantitative), and Category IV (identification), as shown in Table II.
The stability-indicating assay for potency and impurities should physically separate (baseline-resolve) the API, process impurities, and degradation products above the reporting thresholds (RT) (15–16). HPLC method development is not considered a good manufacturing practices (GMP) activity and typically is performed by an experienced separation scientist (6). In contrast, validation of late-stage methods (such as in Phase 3) is considered a GMP activity (1) and is conducted according to a written protocol with predetermined acceptance criteria. A team typically performs method validation, for faster execution.
For new drug development, regulatory agencies have been advocating the use of science-based and risk-based approaches, phase-appropriate method development and validation, and application of quality by design (QbD) principles (7,12,17–18). Phase-appropriate method validation means that early-phase (Phase 1) methods require cursory validation efforts to verify the “scientific soundness” of the method (18–19) (such as the verification of method performance and accuracy with laboratory notebook documentation only). Late-phase methods, however, require full validation in compliance with ICH guidelines (2) with an approved validation protocol and predetermined method performance acceptance criteria.
Also, details of the analytical procedures used in critical quality assessments of clinical trial materials (CTM), including method validation data, must be submitted in regulatory filings, such as Investigational New Drug (IND) applications and New Drug Applications (NDAs). A section on method development can be included in the method validation report. This method development section should also include justifications of the choice of the analytical methods and mode of separation. A complete method development report is also helpful in establishing control strategies for the analytical procedure (6,15).
Method Validation
Parameters: Methodologies and Acceptance Criteria
In this section, the method validation parameters listed in Table I are discussed in detail regarding methodologies and includes examples of acceptance criteria adopted by specific laboratories.
Specificity
Specificity is the ability of a method to discriminate between the critical analytes and other interfering components in the sample. UV detectors are predominantly used in stability-indicating analytical procedures and detect any chromophoric compounds with absorbance at the specified monitoring wavelength. Thus, any coeluted peaks will lead to inaccurate results for these analytes. The specificity of the HPLC method is demonstrated by the physical separation of the APIs from other components such as process impurities, degradants, or excipients (6). During initial method development, forced degradation studies are used to investigate the main degradative pathways and to provide samples with sufficient degradation products to evaluate the ability of the initial analytical procedure to separate the degradation products formed (for example, to demonstrate method specificity) (2, 13). Forced degradation or stress studies may be repeated during late-phase validation.
A typical specificity validation study demonstrates that contaminants or reagents cause no interference; this is done by running a procedural blank and a placebo extract for a drug product method. A placebo is a mock drug product that contains similar amounts of excipients in the formulation without the API. A mixture of API spiked with impurities or degradation products available as reference materials can be used as a “cocktail” or a retention marker solution. This marker solution is useful for further method optimization and can serve as a system suitability test (SST) solution in sample analysis (6,10).
Furthermore, specificity is assessed by a peak purity determination using a photo- diode array detector (PDA) or a mass spectrometry (MS) instrument (example shown Figure 2) (6). In practice, the best secondary “orthogonal” technique generally does not use a totally different separation mechanism, but rather uses another RPLC method with different selectivity (6,7,12). It is beneficial to have an MS-compatible method in early-phase development for peak tracking and rapid identification of unknown peaks (15).
All components of interest should be identified by the observed retention time. Most non-specified impurities are “identified” by their relative retention time (RRT) relative to the API peak (6) for early-phase methods. For complex separations, a retention time marker solution should be included in the SST procedure to reduce the risk of peak misidentifications resulting from retention time shifts (6). If reference materials of impurities are not yet available in early development, a mixed forced-degradation or aged accelerated stability sample (such as one aged for three-months at 40 oC and 75% RH), should be included as an interim substitute in SST to aid in the identification of key analytes.
Accuracy
The accuracy of an analytical procedure is the closeness of the test results obtained by that procedure to the true values. Accuracy studies are usually evaluated by determining the recovery of spiked analytes to the matrix of the sample (such as the diluent for DS and placebo for DP). If a placebo is not available, the technique of standard addition or sample spiking is used. Accuracy must be evaluated at both assay and impurities levels to ensure that the method has acceptable recoveries from nominal placebo concentration that are free from interference.
Method validation for accuracy is typically assessed using a minimum of nine determinations over a minimum of three concentration levels covering the specified analysis range (from independent preparations). The typical range is 80–120% for assay of the API and from the reporting thresholds to at least 120% of the proposed specification limits for impurities and degradation products.
Table III shows a summary of data from a nine-sample study protocol for the simultaneous validation of accuracy, precision, and range of a DP assay methods.
Many organizations have recommendations for acceptance criteria in the company’s standard operating procedures (SOPs). Table IV shows typical acceptance criteria for the validation of accuracy and precision (analytical precision) used by an analytical laboratory for late-phase methods. It uses a sliding scale to allow for higher allowable recovery ranges for low-level impurities (12).
For new chemical entities (NCEs), the impurities may not be identified or specified during early-phase development; thus, they may be monitored using area percent and identified using RRT. Once the project proceeds to the later phases, impurities should be calculated as a weight/weight percent of the active. Accuracy should be studied for impurities that have authentic substances available, and relative response factors (RRF) should be established. For any unspecified impurities, a surrogate reference material with a closely related structure or absorbance can be used for quantitation.
Precision: Repeatability and Reproducibility
Method precision is a measure of the ability of a method to generate reproducible results. The precision of a method is evaluated for repeatability, intermediate precision, and reproducibility. Precision must be evaluated at the assay and impurities levels.
Repeatability is a measure of the ability of a method to generate similar results for a single preparation or multiple preparations of the same sample by one analyst using the same instrument on the same day. There are two types of repeatability, known as system repeatability and analysis repeatability.
System repeatability is determined by multiple injections of the same reference solution (at least five replicate injections). An acceptable level of system repeatability in terms of peak area precision is a mandatory requirement for any quantitative HPLC analysis that will be included in a regulatory submission. Repeatability must be verified by a SST before any regulatory testing can be performed. Traditionally, most laboratories would set a relative standard deviation (RSD) value of <2.0% for peak area precision as a default acceptance criterion. This value is too broad for modern HPLC and ultrahigh-pressure liquid chromatography (UHPLC) autosamplers, which are routinely capable of a precision level of 0.1–0.2%. A more realistic and useful acceptance limit is an RSD of ≤0.73% for n = 5 injections, according to USP <621>.
For late-phase methods, system repeatability must be studied at the quantitation limit (QL) level to ensure reliable precision at this level in the validation study. This precision is accomplished by injecting the QL solution six times and calculating the %RSD. Typical acceptance criteria are peak area RSD ≤10% for six injections with a signal-to-noise ratio (S/N) of ≥10. Tighter acceptance criteria can be set for impurities present at higher concentrations (as shown in Table IV). An injection of a QL concentration is used to verify method sensitivity as part of system suitability testing for an impurity method (6).
Analysis repeatability is assessed for the entire analytical procedure, including sample preparation. It can be evaluated using a minimum of nine preparations, as shown in Table III, or six determinations at 100% of the test concentration. Analysis repeatability is performed by one analyst on one instrument using multiple sample preparations.
The acceptance criterion for analysis repeatability should be set at an RSD of ≤1.0% for the API in DS because of the tight specification, typically 98–102%. Similarly, the acceptance criterion of ≤2.0% RSD of the API in DP is recommended. The acceptance criteria for analysis repeatability for impurities is typically set at ≤5.0% RSD for known impurities and degradation products at 10 times the reporting thresholds (RT), such as those shown in Table IV. The study can be performed using an authentic substance or a surrogate.
Intermediate precision, synonymous with the term ruggedness, is a measure of the variability of method results where samples are tested and compared to those obtained by different analysts, using different equipment and on different days. This study is a measure of intralaboratory variability—the precision that can be expected within a laboratory. Intermediate precision is strongly affected by the design of the protocol (such as how many sources of variance are included) (7). It should be noted that because the method is intended for assay and impurities, intermediate precision should be studied at both assay and impurity levels.
Reproducibility is the precision obtained when samples are prepared and compared between different testing sites. Method reproducibility is often assessed during collaborative studies at the time of technology or method transfer (such as from a research facility to a quality control laboratory of a manufacturing plant or contract manufacturing organization) (7–8).
Sensitivity: Detection Limit and Quantitation Limit
The method detection limit (DL), also known as the limit of detection (LOD) is the smallest amount or concentration of analyte that can be detected. There are several ways to calculate LOD, as discussed in ICH Q2 (R1) (2). The simplest way to calculate LOD is to determine the amount (or concentration) of an analyte that yields a peak height with a S/N of three (6). This can be performed for the materials of specified identified impurities that are available or a surrogate. During validation, the LOD should be verified with at least three injections of the diluted solution to meet at least three times the S/N.
The quantitation limit (QL), also known as the limit of quantitation (LOQ), is the lowest level of an analyte that can be quantitated with some degree of certainty (with a precision of 5–10%) (6). The simplest way to calculate LOQ is to determine the amount (or concentration) of an analyte that yields a peak with a S/N >10. Thus, LOQ is roughly equal to three times LOD. As noted in Table II, the validation of LOQ is required only for stability-indicating methods for the determination of impurities and must be verified by SSTs for each sample sequence. The LOQ must be less than or equal to the reporting threshold (16). It is customary to include a blank, sensitivity solution (by spiking the API at 0.05% or 0.1% level into the sample diluent), and a retention marker solution in the SST sequence to verify method sensitivity and specificity performance (6).
Linearity and Range
The linearity of a method is its ability to obtain test results that are directly proportional to the sample concentration or amount over a given range. For quantitative HPLC methods, the relationship between detector response (peak area) and sample concentration (or amount) is used to make this determination using the external standardization method. Linearity is essential for HPLC methods with UV detection, which uses a single-point calibration with a reference standard solution at 100%. For late-phase methods, a low-level standard (1%) that has a concentration closer to the concentration of the impurities should be used as part of system suitability testing to quantitate the impurities in the samples.
Table V summarizes the typical linearity levels and ranges for late-phase methods, as well as the acceptance criteria for various pharmaceutical method types for comparative purposes (6). For composite stability-indicating assays, linearity validation is conducted at five concentration levels for both API and impurities, and the coefficients of linear correlations are reported. During late-phase validation, the correlation coefficient, y-intercept, slope of the regression line, and residual sum of squares should be determined according to ICH Q2 (R1) (2).
The range of an analytical method is the interval between the upper and lower concentration of a sample that has been demonstrated to show acceptable levels of accuracy, precision, and linearity. For early-phase HPLC-UV methods that use the normalized area percentage (%area), the maximum absorbance of the API peak should be kept <2 absorbance units (AU) to prevent detector signal saturation, which may lead to a failure in method linearity validation (6,15). The range should be determined for assay and impurities before the biobatches (validation batches) are tested.
Robustness
Robustness is a measure of the performance of a method when small, deliberate changes are made to the specified method parameters. Robustness evaluation is used to identify critical parameters for the successful implementation of the method. For early-phase methods, robustness is partially evaluated during method development when conditions are optimized to improve resolution and other method performance criteria (such as specificity, peak shape, sensitivity, solution stability). Robustness must be verified during full method validation before registration; an example is shown in Table VI (6). These factors can be evaluated one factor at a time, or preferably systematically using design of experiments (DoE) (5, 7, 16–17) or other software packages.
Stability of Solutions and Filtration Validation
The stability of solutions should be evaluated during method development to ensure the soundness of the analytical procedure; this evaluation should be conducted systematically as part of the full method validation study before drug product registration.
All sample and reference solutions used in the analysis should have solution stability determined for up to seven days, if possible. This evaluation is essential because solution stability problems can cause inaccuracy when prepared samples cannot be analyzed on the same day or within expiry. Stability and storage conditions should be described in the analytical method. A more extended validation period for a stable API solution is helpful for laboratory productivity because reference solutions may be reused without preparing fresh solutions.
A filtration study for a DP test method should be conducted on at least one globally available filter (such as a disposable 22-mm 0.45 μm syringe filter) (12) if a filter is used. Filtrates collected sequentially from a sample solution spiked with impurities (a mixture solution), and a solvent blank should be analyzed and compared with centrifuged or unfiltered samples of the same solutions to evaluate the recovery of all analytes and to demonstrate that there is no interference from filter contaminants (12). Recommended acceptance criteria for such validation studies from a specific pharmaceutical company are shown in Table VII (12).
Method Validation Approaches and Software Platforms
In this section, current method validation approaches recommended by regulatory authorities are briefly described. Two validation software platforms are also briefly described.
Science- and Risk-Based Approaches in New Drug Development
In recent years, regulatory authorities have endorsed the use of science- and risk- based approaches and the application of QbD with a more systematic exploration of process parameters with DoE and statistical tools (7,12,15). These method validation approaches are described in ICH Q8, Q9, and Q10 (17,18,10) and forms the preamble for ICH Q14 (5).
A Phase-Appropriate Approach to Method Development and Validation
The phase-appropriate approach to method development and validation is described in the second article in this series (15) and elsewhere (7,20–21). The approach applies to method validation studies where more vigorous verification efforts with increasing quality oversight are performed as the new drug candidate progresses to later clinical phases, as shown in Table VIII (7,12). The term method qualification often refers to the process to verify that the performance of early-phase methods is adequate for scientific investigation (this is less arduous than late-stage validation). The term qualification is often used in the context of equipment qualification (19). Note that the U.S. Food and Drug Administration (FDA) considers both terms, method validation and method qualification to be synonymous, because the process of method validation should be phase-appropriate.
Note that the stringent acceptance criteria for method validation according to ICH guidelines recommended for commercial or late-stage drug products may not be appropriate for early-phase methods (7,15,20–21). For early-phase methods, the criteria suggested by the Inter- national Consortium for Innovation and Quality in Pharmaceutical Development (the IQ Consortium), which are shown in Table IX, in the supplementary information online, may be considered (10).
Strategies to Expedite the Method Validation Process
The actual validation process (timing, protocol, and reporting) can vary widely from one company to another and the process is often dictated by internal SOPs. There are no regulatory requirements to use validation protocols for early-phase methods. Nevertheless, many companies have adopted the use of generic method validation plans and reporting templates to ensure better productivity and consistency within the organization. Examples of generic method validation protocols and reporting templates for early-phase clinical trial materials are shown in Tables X to XIII.
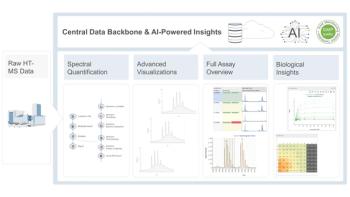
Commercial Software Packages
The application of the principles of QbD in process development with more systematic DoE approaches and statistical analysis can be implemented using off-the-shelf software packages such as Design Expert, JMP, or other software packages (22–23). Two common software tools customized explicitly for the method validation process are mentioned here.
Method Validation Manager (MVM), an optional software package for the Waters Empower 3 Chromatography Data System (CDS) can be used to perform chromatographic method validation, from protocol planning through final reporting. MVM can be used to manage the method validation workflow by designing the studies and documenting results with statistical calculations in Empower 3. MVM is also capable of generating reports using standardized templates and archiving data in a database (24).
The Method Validation Experiment Suite offered by S-Matrix automates method validation through a collection of method validation studies (specificity, filter validation, solution stability, accuracy, linearity, range, precision, and robustness) required by ICH and USP guidance. It performs workflow management by creating standardized workflow templates for executing the studies and facilitating documentation, review, and reporting processes (25).
Method Validation Summary Data from Two Case Studies
Below, we provide two summary validation data tables from an early- and late-phase stability-indicating method to illustrate results from actual validation studies.
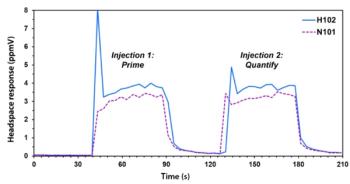
Case Study 1: An Early-Phase (Phase 0) DS Method for an NCE
The first case study comes from the columnist’s own method development project during the early phase of his pharmaceutical career. It illustrates an entire method development and validation case study within two weeks for a pre-IND (phase 0) stability-indicating method for an NCE. The method development process is described in more detail elsewhere (26), and the final method conditions and the chromatogram are shown in Figure 3. The key analytes of this assay are the API, an impurity eluting at ~6.4 min (an isomer of the API), and the immediate synthetic precursor eluted at ~7.6 min.
Table XIV provides a summary of validation results for this stability-indicating composite assay and impurity method. This data set is included to illustrate a real-life validation summary to document the scientific soundness of the method (20, 26). However, the data collected exceeded the typical requirements expected for early development.
Method specificity was demonstrated by resolving all impurities from each other and the API with a focus on two impurities (isomer and the precursor). The evaluation of the peak purity of the API by photodiode array (PDA) peak purity and MS indicated that the API peak is spectrally pure. The MS spectra of the up-slope, apex, and down-slope of the API peak showed no new m/z ion >1% was observed.
Method linearity, accuracy, and precision data collected show acceptable performance for the API and the precursor. A robustness study using DoE software (Design Expert) toward perturbations of variables (column temperature (T), detector wavelength (λ) flow rate (F), gradient time (tG), % trifluoroacetic acid in mobile phase A) showed that the method is robust to these variations. Three columns from different bonding lots were used to demonstrate the robustness of the separation toward lot-to-lot inconsistency.
Case Study #2: A Late-Phase Method for a Complex DP with 4 APIs
Table XV shows the method validation summary data of a late-phase stability-indicating UHPLC method for an antiviral oral combination DP with four APIs, described in detail elsewhere (15, 27).
Summary and Conclusions
This paper provides an updated overview of the validation of stability-indicating HPLC analytical procedures for the determination of the API, impurities, and degradation products in DS and DP. The article describes regulatory requirements, validation parameters, methodologies, and example acceptance criteria for early- and late-phase methods as well as validation trends and software tools. Examples of generic protocols, report templates, and validation data summaries are used to illustrate the typical practices and data collected from these case studies. This installment completes the three-part series devoted to providing the reader with a concise overview of stability studies and the method development and validation of stability-indicating analytical procedures.
Disclaimer
A challenge in writing this overview of method validation lies in the interpretation of the evolving regulatory guidelines and their acceptance criteria, which are highly dependent on the development phase. In addition, the case studies, generic method templates, and data examples in this paper are drawn from published data or company-specific SOPs, which may vary from those used by organizations with a different interpretation of the regulations. The information presented provides an updated overview of common practices to be used as supplemental references. The views presented represent the collective opinions of the authors formed from reviewing the literature and published guidelines and from our own working experience in the pharmaceutical industry. These views bears no relationship to those of LCGC or any other organization.
Acknowledgments
The authors express their gratitude to the following colleagues for their time and effort providing timely reviews of the manuscript to improve the technical content and clarity: Jane Weitzel of Zinata; Jing Capucao of Johnson & Johnson; Alice Krumenaker of TW Metals, LLC; Mark Shapiro of MCS Pharma Consulting; Joshua Ayers of ASQ Solutions; Tamara Andreoli of Medinova AG, Schweiz; He Meng of Sanofi; Hector Rebollo of Prism-A Consulting Services; Kate Evans of Longboard Scientific Consulting; and Matheus Martins of Daichi Sankyo Brazil.
References
(1) Code of Federal Regulations (CFR), Part 211.194(a), Current Good Manufacturing Practice for Finished Pharmaceutical Products (U.S. Government Printing Office, Washington, DC, 2019).
(2) International Council for Harmonization, ICH Q2 R1, Validation of Analytical Procedures: Methodology (ICH, Geneva, Switzerland, 2005).
(3) USP 37/NF 32, General Chapter USP <1225>, Validation of Compendial Methods (United States Pharmacopeial Convention, Rockville, Maryland, 2013).
(4) International Council on Harmonization, ICH Q1A R2, Stability Testing of New Pharmaceutical Products (ICH, Geneva, Switzerland, 2003).
(5) International Council for Harmonization, ICH Q14, Analytical Procedure Development, and Revision of Q2(R1) Analytical Validation (Concept Paper) (ICH, Geneva, Switzerland, 2018).
(6) M.W. Dong, Regulations, System Qualification, Method Validation and Transfer, in HPLC and UHPLC for Practicing Scientists (Wiley & Sons, Hoboken, New Jersey, 2nd ed., 2019), Chapter 11.
(7)H.T. Rasmussen, W. Li, D. Redlich, M. I. Jimidar, in S. Ahuja and M.W. Dong, Eds., Handbook of HPLC in Pharmaceutical Analysis (Elsevier, Amsterdam, The Netherlands, 2005), Chapter 6.
(8)A. Lister, in S. Ahuja and M.W. Dong, Eds., Handbook of HPLC in Pharmaceutical Analysis (Elsevier, Amsterdam, The Netherlands, 2005), Chapter 7.
(9) M. E. Swartz and I. S. Krull, Handbook of Analytical Validation (CRC Press, Boca Raton, Florida, 1st ed., 2012).
(10) D. Kou, L. Wigman, P. Yehl, and M.W. Dong, LCGC North Am. 33(12), 900– 909 (2015).
(11) I. Krull and M. E, Swartz, Validation Viewpoint, LCGC North Am. (regular columns on validation).
(12) H.T. Rasmussen and M.W. Dong, “HPLC Method Development Short Course,” Eastern Analytical Symposium, Somerset, New Jersey, 2004.
(13) International Council for Harmonization (ICH), ICH Q6A, Specifications: Test Procedures and Acceptance Criteria for New Drug Substances and New Drug Products: Chemical Substances (ICH, Geneva, Switzerland, 1999).
(14) ICH, ICH Q10, Pharmaceutical Quality System (Geneva, Switzerland, 2008).
(15) M.W. Dong, K. Huynh-Ba, and J.T. Ayers, LCGC North Am. 38(8), 440–456 (2020).
(16) ICH, ICH Q3A R2, Impurities in New Drug Substance, Q3B(R2), Impurities in New Drug Products (Geneva, Switzerland, 2006).
(17) ICH, ICH Q8 R2, Pharmaceutical Development (ICH, Geneva, Switzerland, 2009).
(18) ICH, ICH Q7, Good Manufacturing Practice Guidance for Active Pharmaceutical Ingredients (ICH, Geneva, Switzerland, 2016).
(19) L. Ng, “Best Practices and Application of GMPs for Small Molecule Drugs in Early Development,” presented in IQ Consortium Workshop, February 4–5, 2014 Washington DC.
(20) Analytical Procedures and Methods Validation for Drugs and Biologics Guidance for Industry (U.S. Food and Drug Administration, Silver Spring, Maryland, 2015).
(21) S.P. Boudreau, J.S. McElvain, L.D. Martin, T. Dowling, and S.M. Fields, Pharm. Technol. 28(11), 54–66 (2004).
(22) J. Anthony, Design of Experiment for Engineers and Scientists (Elsevier, London, United Kingdom, 2nd ed., 2014).
(23) W. Li and H. T. Rasmussen, J. Chromatogr. 1016(2), 165–180 (2003).
(24) Empower 3 Software Method Validation Manager, 720001488 EN, Waters Corporation, Milford, Massachusetts, 2017.
(25) Fusion Method Validation. http://www.smatrix.com/fusion_lc_method_valida-tion.html (accessed August 2020).
(26) M.W. Dong, HPLC Method Development, HPLC and UHPLC for Practicing Scientists (Wiley & Sons, Hoboken, New Jersey, 2nd ed., 2019), Chapter 10.
(27) M. Dong, D. Guillarme, D. Prudhomme, et al., LCGC North Am. 32(11), 868–876 (2014).
ABOUT THE AUTHORS
Michael W. Dong is a principal of MWD Consulting, which provides training and consulting services in HPLC and UHPLC, method improvements, pharmaceutical analysis, and drug quality. He was formerly a Senior Scientist at Genentech, Research Fellow at Purdue Pharma, and a Senior Staff Scientist at Applied Biosystems/PerkinElmer. He holds a PhD in Analytical Chemistry from the City University of New York. He has more than 130 publications and a best-selling book in chromatography. He is an editorial advisory board member of LCGC North America and the Chinese American Chromatography Association. Direct correspondence to:
Kim Huynh-Ba is the managing director of Pharmalytik LLC. (www. pharmalytik.com), which provides consulting services in Stability Sciences, Quality Management Systems, and Analytical Development. She is an Adjunct Professor at Temple University-School of Pharmacy and Illinois Institute of Technology (IIT). Kim is a member of the US Pharmacopeia’s Council of Expert, chairing the Chemical Medicines Monograph IV Expert Committee, USP Good Documentation Practices Expert Panel, USP Organic Impurities of Drug Substance and Drug Products Expert Panel. She is on the editorial board of the AAPS Open, the Journal of GXP Compliance, and the Journal of Validation Technology. Kim has authored ~30 technical publications and the editor of two books on stability testing to support registration in global markets.
Anissa W. Wong is a Sr. Research Scientist working on method development, method validation, and GMP analysis at Gilead Sciences. She was formerly Research Scientist at Theravance and Senior Chemist at ALZA Corporation (J&J Company). She has authored 10+ technical publications.
Articles in this issue
about 5 years ago
How Can We Run a Gas Chromatograph from Anywhere?about 5 years ago
The Importance of Corporate Culture in Ensuring Data Integrityabout 5 years ago
Comparing Scientific Marketing to Analytical RealityNewsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.