Stability Studies and Testing of Pharmaceuticals: An Overview
This instalment is the first in a series of three white papers on stability studies and testing of pharmaceuticals, as well as the development and validation of stability-indicating high performance liquid chromatography (HPLC) methods. The series is co-authored by Kim Huynh-Ba, a subject-matter expert on stability testing and regulatory compliance, and Michael Dong, the columnist on “Perspectives in Modern HPLC”. This first instalment provides a comprehensive and updated overview of stability studies and testing of small molecule drugs, current regulatory requirements, and industry practices for forced degradation, as well as possible approaches for reduced testing and data evaluation to expedite stability study timelines.
This instalment is the first in a series of three white papers on stability studies and testing of pharmaceuticals, as well as the development and validation of stability-indicating high performance liquid chromatography (HPLC) methods. The series is co-authored by Kim Huynh-Ba, a subject-matter expert on stability testing and regulatory compliance, and Michael Dong, the columnist on “Perspectives in Modern HPLC”. This first instalment provides a comprehensive and updated overview of stability studies and testing of small molecule drugs, current regulatory requirements, and industry practices for forced degradation, as well as possible approaches for reduced testing and data evaluation to expedite stability study timelines.
Determining product shelf life is a regulatory requirement for pharmaceuticals and many other regulated consumer products. The shelf life of medicines is set following stringent regulations; therefore, efficient application of stability science is critical. The shelf life (expiration dating or expiry) is displayed on labels of pharmaceutical products to ensure the integrity, quality, and potency of the product when used within that time period. Shelf life is established using data that are generated to verify the label claim, and approved by the regulatory agencies. An expiration date is required by regional laws to ensure the safety, efficacy, and quality of the drug products, and that these criteria are maintained throughout the labelled shelf life of the pharmaceutical product.
Most companies have established standard operating procedures (SOPs) to supplement regulatory guidelines to provide more specific details, and ensure that stability studies are appropriate for their specific product types. Nevertheless, stability programmes and their practices can vary widely, particularly between large and small pharmaceutical companies, often due to depth of knowledge and available resources. The primary aim of this paper is to increase understanding of the science, best practices, and regulatory expectations of stability programmes.
The stability profile, a critical quality attribute (CQA) of a pharmaceutical entity, is based primarily on the physicochemical properties of the drug substance (DS) and drug product (DP). The DS is the active pharmaceutical ingredient (API), with small amounts of impurities and degradation products. A DP typically contains a single DS; when the DP formulation has more than one DS, it is referred to as a combination product. For example, many over-the-counter (OTC) products contain multiple active ingredients. For small-molecule orally delivered DPs, such as tablets or capsules, a typical expiration period is two to five years under room temperature storage. Table 1 summarizes the characteristics of stability studies and testing. Each is discussed further in this paper.
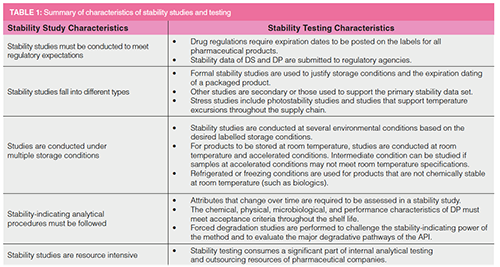
In this paper, we use solid oral dosage forms, such as tablets or capsules, as examples. Four types of testing for orally available products, listed in Table 2, are discussed. Biological products are not covered here.
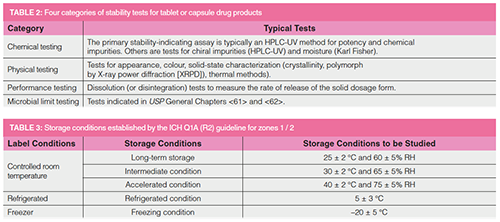
Other dosage forms such as parenterals also have similar types of tests, including identity, chemical testing (assay and impurities), physical testing (pH, clarity, particulates), and sterility tests as appropriate.
Stability Studies in New Drug Development
During drug discovery, the medicinal chemist focuses on synthesizing new chemical entities (NCEs) that interact selectively with the molecular targets (such as receptors or enzymes), leading to potential disease mitigation (1). The structural motifs of a leading NCE candidate are then optimized for biological activities and safety by the synthesis of a series of analogues. The optimization tools include in vitro and in vivo animal studies (such as biochemical target binding, biomarkers, or animal models), bioavailability (pharmacokinetics), and toxicological evaluations (1,2). The desired NCEs need to be reasonably stable to be viable drug candidates, which are scaled up for clinical trials using simple formulations. Eventually, the final DS is formulated into a commercial drug product, and submitted for regulatory approval.
In most pharmaceutical companies, the nomination of an NCE to the status of a drug development candidate triggers the formation of a multidisciplinary technical development team. This team is responsible for taking the drug candidate into clinical trials in humans, and eventually to drug approval, production, and commercialization. The team is responsible for activities referred to in regulatory documents under the heading of “Chemistry, Manufacturing, and Control” (CMC), and thus the team is often called the CMC team.
Stability studies for clinical trial materials (CTMs) are conducted to monitor their CQAs and help identify which formulation will result in a successful candidate for regulatory submission. In the United States, an expiration date is not required on the label of a CTM, but this is required in many countries, such as those in Europe. Forced degradation studies (also referred to as stress studies) are used to challenge the stability-indicating power of the analytical method. The accelerated studies, which require storage under higher temperature and humidity compared to normal room-temperature conditions, allow the samples to degrade at a faster rate. Data from accelerated studies may be extrapolated to project the results of a longer-term, controlled-room-temperature study. Most pharmaceutical products exhibit a linear degradation trend. Based on the stability data, a retest period is assigned to the DS, and an expiration date to the DP.
The CMC team typically consists of scientists from various functions, such as process chemistry (synthetic organic chemistry), formulation (pharmaceutics), analytical chemistry (analytical development and quality control [QC]), pharmacokinetics and drug metabolism (PKDM), outsourcing, regulatory affairs, supply chain, and project management. The degree of involvement depends on the development phase. For example, the analytical development chemist is more involved in the discovery and earlyâphases of development to support DS and DP processes. In contrast, quality control chemists and regulatory staff are more active in the later clinical phases for CTM manufacturing and regulatory filings (3,4). Some of the team activities include:
- Conducting the necessary synthetic process scale-up of the DS (process chemistry staff)
- Performing detailed characterization of the API, developing and validating analytical procedures for DS and DP, and identification of critical impurities and degradation products (analytical development staff)
- Finding the optimum solid-state form (salt, crystallinity) or polymorph of the API (analytical staff)
- Conducting stability studies to support clinical development and registration (analytical and QC staff)
- Designing and developing processes for formulations of CTMs and the final commercial DP (pharmaceutics staff)
- Setting acceptance criteria for CQAs (specifications) to monitor clinical quality and establishing commercial specifications (QA and regulatory staff)
- Manufacturing CTMs (CMC team and outsourcing and project management staff)
- Assembling the CMC submission package for regulatory filings (CMC team and regulatory staff).
In this series of white papers on stability testing, we focus on the tasks performed by the analytical development and QC scientists within the CMC team. The first task for the analytical chemist assigned to the CMC team is to develop a reasonable stability-indicating method for monitoring the quality of CTMs. This method is typically a “composite” analytical procedure that determines both the potency of the API and chemical impurities of the DS. Ideally, it can also be used for the assessment of DP samples. Once a feasible analytical procedure is established, forced degradation studies are performed to evaluate the specificity of the analytical procedure. This method is used in the release testing of the early clinical batches and testing of samples from initial stability studies to support clinical trials (3–5).
The stability-indicating assay and impurities method is typically a gradient reversed-phase high performance liquid chromatography (HPLC) method with UV detection that can separate the API and all the known impurities and degradation products (5). This method is validated to ensure adequate analytical performance (specificity, linearity at 100% target concentration and expected impurities concentrations, accuracy, precision, sensitivity, and solution stability) for “formal stability studies” (defined as studies conducted under Good Manufacturing Practices [GMP]) supporting the establishment of expiration dates for regulatory filings (5,6). Details on the development and validation of the stability-indicating methods will be covered in the second and third instalments of the series. Forced degradation and stability studies are discussed in later sections here.
A better understanding of stability studies and their regulatory requirements is essential for the analytical chemist for several reasons (6,7). First, these studies require many different tests (shown in Table 2) on multiple batches stored at different storage conditions and pulled at numerous time intervals. Second, the process development or formulation scientists may request many experimental batches of DS or formulations to be placed on stability, leading to redundant testing, bringing little added value if not managed with a science- and risk-based approach. Therefore, a better understanding of the design, intent, and best practices of stability studies and a proper interpretation of associated regulations can lead to more efficient implementation of stability programmes.
Objectives of this Article
In this instalment, we discuss:
- Regulations and regulatory expectations of stability programmes
- The goals of forced degradation studies and examples of forcedâdegradation protocols
- A strategy for conducting stability studies to expedite regulatory filings
- Modern predictive stability software tools and statistical approaches to expedite stability studies in a science- and risk-based approach.
- Regulations and Regulatory Expectations of Stability Programmes
- Stability is a Critical Quality
Attribute for Pharmaceuticals
In the Quality by Design (QbD) approach, CQAs describe the properties or attributes pertinent to product quality (8–11). For pharmaceutical products, CQAs are characteristics that impact the safety and efficacy of drug products. Acceptable limits or product specifications must be established and verified by release testing (11). Stability studies of DS and DP are conducted throughout the drug development process, from the preclinical stage to final product approval, with the study size dependent on the phase of development. The initial analytical development activities include the development of analytical procedures, establishment of acceptance criteria, forced degradation studies, DS and DP method validation, and stress tests (3,4,12). In early phases, stability studies may be conducted under limited accelerated conditions, and often without a fully validated suite of analytical methods. CTMs are released against a set of acceptance criteria (such as specifications) for clinical use by the Quality Assurance (QA) group.
Once a product proceeds to Phase 3 development and preparation for product registration, GMP regulations must be followed for finished pharmaceutical products starting from the registration batches (13). The registration batches and commercial products destined to be distributed for patients’ use must undergo stringent release testing by QC to meet the established commercial specifications for identity, purity, potency, and quality of the finished product. While QC performs release testing of the registration batches and issues a Certificate of Analysis (CoA), it is officially released and signed-off by the QA group (or by a “Qualified Person” [QP] in European Union pharmaceutical regulation) for market distribution after receiving approval. A portion of the registration batches is generally used for “formal (registration) stability studies”, and upon commercialization, stability samples are evaluated annually in marketed product stability programmes.
Stability testing of CTMs typically includes tests for appearance, identification and quantification (assay), impurities, dissolution (for solid dosage forms), moisture, and additional physical characterizations such as X-ray powder diffraction (XRPD) tests for crystallinity and polymorph form. This set of tests (customized for the specific DS or DP, or compendial tests) is documented in the product specifications. They must be used to assess the identity, physical form (colour, size, and crystallinity), purity (chemical and chiral purity) (3,4), water content, performance (dissolution), and microbial activity (4,14,15), to ensure that drug quality is maintained throughout the stability studies.
In a stability study, representative batches of pharmaceuticals are stored in controlled stability chambers at different temperatures and relative humidity (RH) levels in proposed packaging (containers, closure systems) (6,7). These storage conditions represent long-term, accelerated, or stress storage conditions. Samples are periodically removed from these chambers according to a pre-approved schedule, and tested to verify that the pharmaceutical products meet specifications within the established expiration date under the recommended storage and packaging conditions. Formal stability testing to support regulatory filings must be conducted with validated methods according to GMP regulations (13,16). These stability data are also used to support the manufacturing, registration, shipping, and transportation of commercial products. Furthermore, stability data are collected through clinical formulation phases, process development, proposed packaging selection to establish the drug product’s shelf life, storage conditions, and commercial specifications.
Post-marketing studies are conducted to verify that any changes to raw material, manufacturing steps, or container or closure systems have not affected the DP through its expiration date based on product commitment. Any planned change of raw material, manufacturing, or packaging must be evaluated to determine if additional stability studies or regulatory filings are needed.
The United States Food and Drug Administration (FDA) has determined that the stability profile is a critical attribute of a pharmaceutical product. Therefore, stability studies are necessary to support any submission such as an Investigational New Drug (IND), New Drug Application (NDA), or Abbreviated New Drug Application (ANDA) filing (1). The stability data packages within the CMC section are typically the most extensive non-clinical sections in these submissions. They include tabulated data, graphs, narratives to summarize the stability profile of the packaged product to justify specifications, and proposed expiry for the product.
Harmonization of Regulations: ICH Quality Guidelines for Stability Studies
Given that stability testing is expensive and labour-intensive, it is imperative to understand the regulatory requirements and their intent to avoid unnecessary studies. In addition, regulations vary significantly from country to country, which impacts the cost of new drug development and the registration timeline for a global product launch. Therefore, in the early 1990s, the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH), consisting of representatives from regulatory agencies and scientists from pharmaceutical industries, was formed. The council’s role is to harmonize the quality requirements for pharmaceuticals to minimize redundant testing, and reduce the time and cost of new product development. The ICH stability guideline, ICH Q1, was the first quality guideline established by the council, indicating the significant need for harmonization of global stability requirements.
The ICH initially harmonized three geographic regions: the United States, the European Union, and Japan, which encompassed Zone 1 and Zone 2 of the World Health Organization (WHO) climatic zones. However, many countries outside Zone 1 and 2 joined the ICH, or voluntarily adopted these guidelines later with various modifications. The current stability guideline (Q1A [R2]) harmonized the storage conditions, frequency of required testing, and the minimum amount of data needed for registration (6–8). Table 3 lists the stability storage conditions established by ICH Q1A (R2) (8).
Forced Degradation Studies
Forced degradation studies, or stress testing, are required by regulations and scientific necessity during the initial method development process, according to ICH Q1A (R2) and ICH Q2 (R1) (8,16). Although regulations mandate that these studies must be performed, the guidance does not provide directions on procedures or conditions to use. The actual protocols employed appear to vary widely in different organizations. An overview of the chemistry fundamentals of drug forced degradation studies and best practices can be found in books, articles, and other resources (17–20).
Forced degradation studies are performed to investigate the major degradative pathways of the DS and DP and support the initial development of the DS stability-indicating methods (3,5,12). High-stress conditions are employed to subject DS and DP to conditions more severe than accelerated conditions to serve several purpose:
- To rovide insight into the degradation pathways of DS and DP and their mechanisms, facilitating the development of stable formulations and selection of suitable packaging
- To obtain samples to verify method specificity and structure elucidation of significant degradation products
- To allow the differentiation of impurities and degradation products from the DS, excipients, and other interference
- To facilitate the rapid establishment of CQAs for selection or elimination of selected testing.
- To rapidly identify any excipient incompatibility issues with the DS
- To generate potential data to support the justification of specifications.
Forced degradation studies are conducted under high temperature, humidity, acid/base, oxidative, and light conditions in both solid and solution states. Table 4 lists an example set of stress conditions for DS. An important goal of forced degradation studies is to generate a potential level of degradation products that may form during manufacturing and on stability storage. Typically, forced degradation studies are conducted until a 5–20% loss of API is observed (18,19). This range is set to produce a reasonable amount of degradation products to facilitate method development and to avoid secondary degradation products from an unstable degradant (which are not observed under actual stability conditions). It should be noted that the conditions should be selected based on the physicochemical properties of the individual DS and DP.
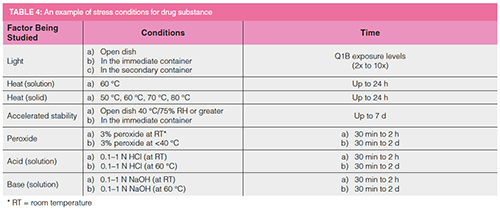
Thermal Degradation
The effect of temperature is studied by exposing the drug substance to high temperatures in increments of 10 oC from 50 to 80 oC. Thermal degradation is the primary degradation pathway of the DS in the solid state.
Solution State Acid/Base Degradation
Solution-state degradation mechanisms may be different, and should also be explored.
If the drug substance is not soluble under aqueous conditions, then a small amount (up to 10%) of organic solvent (acetonitrile or methanol) can be used to solubilize the DS, and the acid or base can then be added to stress the samples. Attention should be given to the functional groups present in the drug molecule when selecting a co-solvent (20).
It is not advisable to use a high concentration of acid or base, because doing so is neither practical nor necessary. A few papers have suggested a series of extensive steps of pH changing from pH 2 to pH 10 buffer. It may not be necessary as a routine practice, unless for a specific DS or as part of a stress Design of Experiments (DoE) to establish a stability model (22).
Photostability
Photostability studies are essential, and must be performed to generate primary light-induced degradation products by subjecting one representative batch of the DS to the light exposure listed in ICH Q1B. The standard light exposure is 1.2 million lux hours of visible light and 200 lux hours of near UV, with storage conditions controlled at room temperature.
These studies can be repeated when there is a change of DS samples, such as a new synthetic route, with different crystallinity form, different supplier, or a change of DP formulation.
During the method development phase, forced degradation samples are typically evaluated using a preliminary mass spectrometry (MS) compatible HPLC method with a photodiode array detector (PDA) to collect information on peak area under the curve. The MS and PDA data are used for peak tracking, peak purity assessment, identification of degradation products, impurities, and interferences (3,5,19).
Table 5 shows an example of a more extensive, elaborate forced degradation protocol used by a pharmaceutical laboratory to collect data for most of their NCEs using a four-temperature thermal stressing condition matrix (ambient, 60 oC, 70 oC, 80 oC) for acid, base, oxidative, light, humidity, buffered solution, and prolonged stressed duration (up to 21 days). This sample-intensive protocol was made feasible by this centralized and automated laboratory specializing in supporting forced degradation studies for the development site. The laboratory utilized automated sample storage and retrieval system called “Powderium” (a powder dispensing workstation), robotics, programmable liquid handling, and refrigerated storage of quenched samples (18,19).
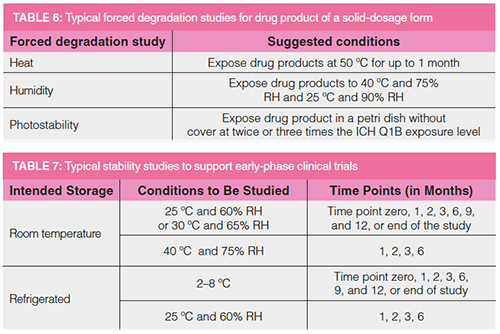
Table 6 provides a summary of forced degradation studies performed on solid dosage forms. Note that acid, base, and oxidative exposures are not used, because these conditions are not representative of realistic storage or exposure situations. The length of exposure should be evaluated carefully, depending on the dosage forms or the formulation. For example, capsule formulations or film-coated tablets may not be able to withstand a temperature higher than 60 oC for an extended length of time.
Similar to the DS, a goal of 5–20% loss of active ingredient is recommended. If DS or DP is stable and the desired degradation level cannot be reached under high-stress conditions, studies should be terminated. Overstressing a sample may lead to secondary degradation products that are not present in formal stability studies. In contrast, understressing may lead to insufficient degradation products for method development or identification (12). For each condition of the forced degradation study, the chromatogram is compared with that of a control sample to document the mass balance of the API (% loss of API) and % degradation (normalized peak area %). For all conditions, the peak shapes and peak purity (by PDA and MS) of all components should be assessed for coelution or presence of interferences (3–5).
Accelerated and stress studies are performed to induce quicker degradation than would be observed in recommended storage conditions. Results from these studies are used to estimate the stability profile of the DS and DP at long term storage conditions, establish the actual degradation pathways, and demonstrate the intrinsic stability of the DS. It is recommended that these studies be implemented under GMP conditions because the results of these studies may be used as supporting information in regulatory document packages. Full shelf-life studies are still needed to verify the retest date of the DS and expiration date of the DP.
While discussions on forced degradation studies for NCEs in NDA applications are generally plentiful, those for ANDA are often insufficient and may result in regulatory deficiencies. For instance, the impurity profiles may not be completely derived or sufficiently discussed (20). In addition, the labelling for generic drug products should be concordant with that of the reference listed drug (RLD) and with a compendial monograph, as applicable (20).
Stability Storage
Stability samples are kept in a controlled temperature in humidity stability chambers. The ICH Q1A (R2) guideline requires that these chambers be controlled within ±2 °C and ±5% RH for chambers operated at 25 °C/60% RH, 30 °C/65% RH, and 40 °C/75% RH. The refrigerated condition is controlled at 5 °C ± 3 °C (2–8 °C) with ambient humidity (monitored but not controlled). These chambers are equipped with sensors for the continuous monitoring of temperature and relative humidity. These data are captured electronically or by chart recorders with backup power. Excursions will be noted with an alarm system. When the chambers are out of tolerance (see above), investigations must be performed to identify the cause of the issue and determine the impact of the stored samples (7).
The stability chambers are fully qualified and maintained, and their access is limited to authorized personnel to ensure that sample removal is tracked and controlled. Maintenance and service records must be available for inspection during audits. Downtime must be limited, and a backup plan must be developed to avoid issues that can affect sample storage and data integrity. An annual chamber inventory programme is also necessary to track the sample storage and disposition at any time.
Stability Study Strategies to Expedite “First-in-Human” Clinical Trials
Minimizing “Time to Market” is an essential strategy for most pharmaceutical companies (1). Given that regulatory agencies expect to see three months of stability data in IND filings to enable Phase 1 clinical trials, it is customary to perform preliminary accelerated stability studies on the Good Laboratory Practices (GLP) toxicological DS and prototype DP batches to provide supporting data for quicker IND submissions. Early-phase stability studies are typically short, as shown in Table 7, and the study conditions depend on where the clinical trials will take place. During Phase 1, the analytical procedures are usually not fully validated, though specificity, accuracy, linearity, and precision studies should be completed. These time-saving strategies allow the pharmaceutical companies to start Phase 1 clinical trials as soon as possible after the nomination of the drug candidates.
Characterization studies of the API and DP continue during formulation development. It is recommended that the forced degradation studies be repeated before the release testing and the initiation of the formal stability studies under GMP regulations and ICH Q1A (R2) guideline (8). Examples of standard stability protocols that are listed for different dosage forms at different drug development phases are discussed elsewhere (6,7). Results of the formal stability studies used to determine the drug products’ expiration are included in the stability section of the NDA or ANDA.
Predictive Tools to Establish Product Expiry
Stability data are used to establish the expiry of finished products according to US FDA Good Manufacturing Practices regulation 21 CFR 211.137 (21). The data from the accelerated condition are used to determine a tentative expiration date, but testing at full shelf life is necessary to confirm the approved expiry.
In this section, we discuss examples of useful software tools and statistical approaches to evaluate stability data and to expedite stability studies for establishing product expiry.
Most tools are science- and risk-based, and have a robust statistical underpinning that conforms to the principles of QbD and DoE, which are endorsed by regulatory agencies for pharmaceutical development (9).
Modern Predictive Methods and Approaches
One widely used approach is the Accelerated Stability Assessment Program (ASAP), which uses a modified Arrhenius approximation. This approach uses degradation kinetics at a few stressed conditions in 1–2 weeks, and extrapolates to lower temperatures and humidity for longer timeframes. The advantages of this strategy are that the length of these experiments is short and the experiments use fewer resources. The accuracy of this model assumes a first-order reaction, which is often the case for hydrolysis-based degradation (6,22). The disadvantage is that the presumed kinetic model limits the degradation to less than a percent and requires extrapolation of three factors simultaneously: time, temperature, and humidity. These disadvantages are minimized when the DS and DP have a simple kinetic pathway, and the primary stability drivers are temperature and humidity (23). Another drawback could occur when the kinetic route is complex or nonlinear or involves physical changes, which may result in the linear model not being accurate. Recently, this approach was also used to select appropriate packaging based on its thermal and moisture-barrier characteristics, and to optimize the drug:excipient ratio of the formulation based on the moisture content (22). This approach has gained popularity, mainly to set expiry for clinical materials, and has been accepted by multiple regulatory agencies (24).
Another successful tool is the Predictive Characterization Study (PCS), a rapid development of robust stability models using a semi-empirical design space. It is a systematic study that evaluates the product data of samples exposed to a series of storage conditions to build predictive stability models to establish the design space and control strategy based on the QbD concept, such as setting specifications and selecting proposed container–closure systems. This approach is also found acceptable by many regulatory agencies (23–25).
Improved modelling tools have enabled stability predictions with accelerated timeframes compared to those of the traditional extrapolation approach. Besides providing a more accurate way to justify an expiry assignment, these models are used to increase the understanding of the critical factors that influence the quality of the DS and DP, as demonstrated in empirical science and risk-based approaches detailed in ICH Q8–Q11. These approaches are often utilized by large pharmaceutical companies with better modelling resources and expertise. A regulatory template has been shared to standardize on critical elements to use risk-based predictive stability data for setting up shelf life to support clinical development (26).
Trending Analysis
The purpose of the stability programme is to establish a retest period for DS or shelf life for DP that will apply to all future commercial batches. Stability data of CQAs of individual batches should remain within specification throughout the assigned retest period of the DS or shelf life of DP. Therefore, the trending of all stability data is very important. Most degradation trends of API are linear; however, the degradation pathway could be a linear, quadratic, or cubic function. The typical ICH Q1E approach for the determination of shelf life through the analysis of data based on a quantitative attribute that is expected to change over time is to determine the period of time at which the 95% one-sided (or two-sided) confidence limit for the mean curve intersects the acceptance criterion (27,28). The annual commitment lots should also be evaluated against the product trend to assure the consistency of the stability profile of the DP and verify if there is any unintended change that may impact the DP.
Reduced Testing with Bracketing and Matrixing
Conducting stability programmes is expensive and time consuming. To reduce costs and increase the efficiency of the stability programme while maintaining regulatory compliance, many companies employ bracketing or matrixing options that reduce the amount of testing and resources required (6,7). ICH Q1A (R2) and ICH Q1D are guidelines to refer to when reduced testing is applied. Although the bracketing and matrixing concepts are included in multiple global stability guidelines, limited numbers of published applications can be found. It is even more challenging to provide examples for the matrixing for an NCE. Here, we explain the similarities and differences between these approaches to illustrate this application.
Bracketing
Bracketing refers to a study design in which only the extreme variables, such as extreme strengths, container sizes, or container fills, are tested. The plan assumes that the stability behaviours of products manufactured or packaged at these extreme levels (such as, for example, highest vs. lowest strength, or largest vs. smallest package size) encompass and represent the stability behaviours of products of the intermediate levels, eliminating the need for testing at the intermediate levels. A bracketing schedule can be applied to multiple strengths of identical or closely related formulations.
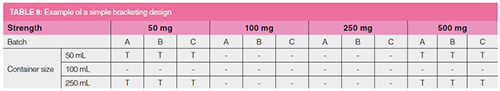
Table 8 shows an example in which the 100 mL container size is bracketed by the 50 mL and 250 mL container sizes; thus, stability samples stored in the 100 mL containers are not tested. Similarly, the 100 mg and 250 mg tablet strengths are bracketed by the 50 mg and 500 mg strengths. Assuming that the stability profiles of these different strength formulations are the same and the compositions of these tablets are similar, regardless of strength, then the testing of 100 mg and 250 mg tablets may not be needed. ICH Q1A (R2) requires that three batches (A, B, C) be made available for submission. According to the guidelines, a pharmaceutical company could reduce its testing from potentially 36 configurations to only 12 configurations, resulting in significant savings of resources and time (6,7).
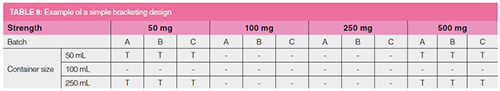
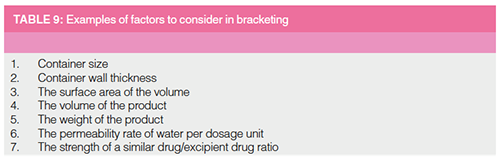
Table 9 lists some factors to which a bracketing approach can potentially apply, assuming that the container–closure system and the headspace of the containers do not have any impact. The disadvantage of the bracketing concept is that when one of the results is out-of-specification, all bracketed configurations data could then be at risk. Full testing would need to be activated mid-study, complicating the data set, and negating the benefit of any testing reduction. In addition, all bracketed factors (for example strengths/formulations and package configurations) will need to be registered in all end markets, even if only a subset will be commercialized. Due to the risk, the bracketing concept is used more often for post-approval or annual product monitoring stability studies rather than for DPs from NCEs.
Matrixing
Matrixing is a statistical design of the stability schedule in which a selected group of samples of the total number of possible samples is tested at a specific time point. At the next time point, a different group should be tested. At each time point, the stability data of that group of samples will represent the stability of the whole set of studies.
Similar to the bracketing approach, this design also assumes that all the batches have similar stability profiles; thus, there is no need to generate all the results. The long-term trends of all configurations are approximately linear across the whole set of all studies, and the comparative stability of each presentation can be evaluated with the reduced schedule. Many options are available with the matrixing concept, which could reduce the testing schedule by a third, a half, or two thirds, depending on the aggressiveness of the statistical extrapolations and risk assessment for the design (6,7).
Table 10 shows an example of a two-thirds factorial matrixing design. In this schedule, there are two strengths and three batches made of each strength. All presentations are tested at time zero, 12 months, and the end of the study (36 months) for the highest possible precision as these time points are critical to the DP stability profile. For all other time points (3, 6, 9, 18, and 24 months), only two-thirds of the presentations get tested at a rotating schedule. Therefore, all configurations are tested at different time points for the same amount of times in total.
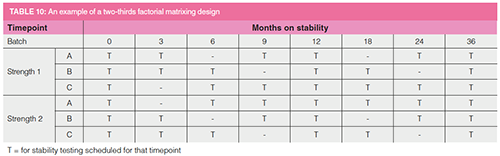
The matrixing approach requires that all samples be placed in stability chambers, including at the timepoints that are reduced. Therefore, when there is an instability issue, the testing schedule can be changed to test all configurations. If some data points are not available, there will be a minimum impact on the entire study of multiple presentations.
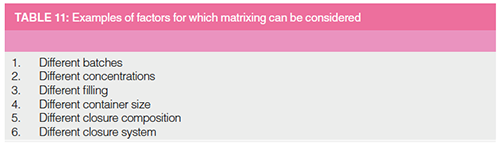
Table 11 lists some examples of factors where matrixing can be used to reduce testing. Matrixing also provides more flexibility because different reduced testing options can be performed for various tests depending on the testing confidence. Realistically, matrixing should be used only for label storage conditions. The accelerated stability data may provide some insight into the stability profile of the product at the label storage conditions. Because matrixing is a statistical concept, evaluation of data can be more involved, and assessment of all the presentations as a complete set is more complicated, which explains why this approach is not used widely. These reduced testing approaches are discussed in detail in many global guidelines; however, a lack of knowledge of matrixing among regulatory reviewers and internal quality and regulatory professionals may hinder the use of this application to reduced stability testing.
Stability Reports and Regulatory Submissions
Stability reports are required in all phases of regulatory submissions regardless of lifecycle state (such as NDA, ANDA, or supplement NDA). The stability database comprises laboratory data generated and stored electronically or as printed reports. These stability data are entered into stability reports, which are essential to communicate information internally for audit purposes, product investigations, justification of specifications, to support product development, or simply as a communication tool. All detailed information in the report must be verified for accuracy. For an NDA or ANDA submission, the stability report is typically the most extensive non-clinical section to summarize the stability data of the product during its shelf life (6,28).
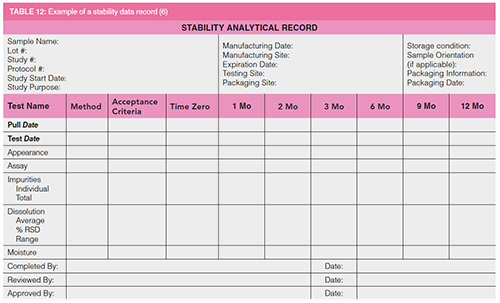
Stability data can be presented in a tabular format, in a graphical representation, a narrative, or a combination of formats. Table 12 is an example of a stability data record. The data tables can be generated manually in a document or printed out from a laboratory information management system (LIMS) or stability management software. All information and data must be reviewed and verified. The conclusion of the stability report discusses whether the data indicate that the product continues to meet the quality specifications or acceptance criteria established for the study and whether the data support the proposed or approved expiration dating period (6,7).
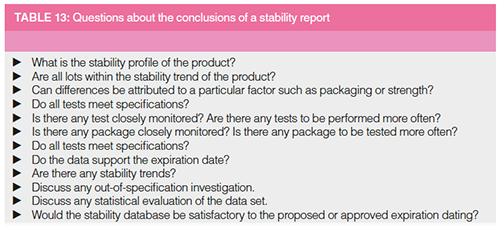
Stability reports should include a statistical evaluation of the currently available data and a discussion of the results according to ICH Q1E or statements that no overall trends and little variability are observed in the dataset. Table 13 lists typical questions that should be addressed in the stability conclusion. “Poolability” of different batches should be evaluated to determine the consistency of the representative stability data and trends with respect to the manufacturing process and analytical method, by comparing the intercepts and the slopes of all batches (6,7,24).
Summary and Conclusions
A robust and science-based stability programme is required for the registration and commercialization of any pharmaceutical product. Regulations in this area are well established; however, the application and interpretation of the regulations vary between companies and regions. ICH harmonizes the main regions to help companies use a standardized approach.
This article provides a high-level summary of regulations and regulatory expectations of stability programmes. It reviews the goals and practices of forced degradation studies to generate sample data to confirm method specificity. A strategy for conducting accelerated stability studies on preliminary batches to expedite initial regulatory filing is described. Finally, predictive stability software-based and statistical approaches such as trending, bracketing, and matrixing are explained.
Acknowledgements
The authors express their gratitude to the following colleagues for their time and efforts to provide timely reviews of the manuscript to improve content accuracy and clarity: Jane Weitzel of Zinata; Jing Capucao of J&J; Mike Shifflet of Johnson and Johnson Consumer Health Care; Adrijana Torbovska of Farmahem; Alice Krumenaker of TW Metals, LLC; Mark Shapiro of MCS Pharma Consulting; Madhavi Mahavadi of BioMarin Pharmaceuticals; Joshua Ayers of ASQ Solutions.
References
- R.G. Hill and H.P. Rang, Eds., Drug Discovery and Development: Technology in Transition (Churchill Livingston, Elsevier, Edinburgh, Scotland, 2nd Ed., 2012).
- M.W. Dong, Drug Development Process, Short Course presented at Pittcon, Philadelphia, Pennsylvania, March 2019.
- M.W. Dong, LCGC North Am.33(11), 764–775 (2015).
- D. Kou, L. Wigman, P. Yehl, and M.W. Dong, LCGC North Am.33(12), 900–909, (2015).
- M.W. Dong, HPLC and UHPLC for Practicing Scientists (John Wiley & Sons, Hoboken, New Jersey, 2nd Ed., 2019), Chapters 9–11.
- K. Huynh-Ba, Ed., Handbook of Stability Testing of Pharmaceutical Products: Regulations, Methodologies and Best Practices (Springer, New York, 2009).
- K. Huynh-Ba, Ed., Pharmaceutical Stability Testing to Support Global Markets (Springer, New York, 2010).
- International Council for Harmonisation, ICH Q1A (R2), Stability Testing of New Pharmaceutical Products (ICH, Geneva, Switzerland, 2003).
- International Council for Harmonisation, ICH Q8(R2), Pharmaceutical Development (ICH, Geneva, Switzerland, 2009).
- International Council for Harmonisation, ICH Q3A(R2), Impurities in New Drug Substance, ICH Q3B(R2), Impurities in New Drug Products (ICH, Geneva, Switzerland, 2006).
- International Council for Harmonisation, ICH Q6A, Specifications: Test Procedures and Acceptance Criteria for New Drug Substances and New Drug Products (ICH, Geneva, Switzerland, 1999).
- H. Bruemmer and N. Belikova, Pharm.Technol. 41(9), 46–52 (2017).
- 21 Code of Federal Regulations (CFR), Part 211.194(a), Current Good Manufacturing Practice for Finished Pharmaceutical Products (US Government Printing Office, Washington, DC, 2019).
- United States Pharmacopeia Convention, USP 37/NF 32, General Chapter USP <1225>, Validation of Compendial Methods, (United States Pharmacopeial Convention, Rockville, Maryland, 2013).
- United States Pharmacopeia Convention, USP 37/NF 32, General Chapter USP <1226>, Verification of Compendial Procedures (United States Pharmacopeial Convention, Rockville, Maryland, 2013, revised 2018).
- International Council for Harmonisation, ICH Q2 (R1), Validation of Analytical Procedures: Methodology (ICH, Geneva, Switzerland, 1996, updated 2015).
- S.W. Baertschi, K.M. Alsante, and R.A. Reed, Eds., Pharmaceutical Stress Testing: Predicting Drug Degradation (CRC Press, Boca Raton, Florida, 2nd Ed., 2011).
- H.T. Rasmussen, W. Li, D. Redlich, and M.I. Jimidar, HPLC Method Development, In Handbook of HPLC in Pharmaceutical Analysis, S. Ahuja and M. W. Dong, Eds., (Elsevier, Amsterdam, 2005), Chapter 6.
- M.W. Dong and H.T. Rasmussen, HPLC Method Development Short Course, Eastern Analytical Symposium, Somerset, New Jersey, 2004.
- R. Maheswaran, Pharm. Technol. 36(5), 1–6 (2012).
- 21 Code of Federal Regulations (CFR), Part 211.137, Current Good Manufacturing Practice for Finished Pharmaceutical Products (US Government Printing Office, Washington, DC, 2019).
- K. Waterman, Understanding and Predicting Pharmaceutical product Shelf life, In Handbook of Stability Testing of Pharmaceutical Products: Regulations, Methodologies and Best Practices (Springer, New York, 2009), Chapter 6.
- K. HuynhBa et al., Meeting Report, Analytical Approaches to Ensure Product Quality – AAPS Joint Face-to-Face Meeting of the Stability, the Pharmaceutical Impurities, and the CMC Statistics Focus Group, AAPS Open 3 (1), 2017. https://aapsopen.springeropen.com/articles/10.1186/s41120-017-0011-z
- H. Williams et al., Pharm. Technol.41(3), 52–57 (2017).
- D. Lavrich, Rapid Development of Robust Stability Models Using Semi-Empirical Design Space, AAPS Webinar, March 24, 2016. https://aapsopen.springeropen.com/articles/10.1186/s41120-017-0018-5#article-info
- H. Williams, Pharm Technol.42(8), 42–47 (2018).
- WHO Expert Committee on Specifications for Pharmaceutical Preparations Fifty-second report, annex 10, Stability testing of active pharmaceutical ingredients and finished pharmaceutical products (World Health Organization, 2018).
- International Council for Harmonisation, ICH Q1E, Evaluation of Stability Data (ICH, Geneva, Switzerland, 2003).
Kim Huynh-Ba is the managing director of Pharmalytik LLC. (www.pharmalytik.com), which provides consulting services in Stability Sciences, Quality Management Systems, and Analytical Development. She is an Adjunct Professor at Temple University’s School of Pharmacy and Illinois Institute of Technology (IIT), USA. Kim is a member of the US Pharmacopeia’s Council of Experts, and the chair of the Chemical Medicines Monograph IV Expert Committee, USP Good Documentation Practices Expert Panel, USP Organic Impurities of Drug Substance and Drug Products Expert Panel. She is on the editorial board of AAPS Open, the Journal of GXP Compliance, and the Journal of Validation Technology. Kim has authored ~30 technical publications and is the editor of two books on stability testing to support registration in global markets.
Michael W. Dong is a principal of MWD Consulting, which provides training and consulting services in HPLC and UHPLC, method improvements, pharmaceutical analysis, and drug quality. He was formerly a Senior Scientist at Genentech, Research Fellow at Purdue Pharma, and Senior Staff Scientist at Applied Biosystems/ PerkinElmer. He holds a PhD in Analytical Chemistry from City University of New York, USA. He has more than 100 publications and a best-selling book in chromatography. He is an editorial advisory board member of LCGC North America and the Chinese American Chromatography Association. Direct correspondence to: amatheson@mjhlifesciences.com
Detecting Hyper-Fast Chromatographic Peaks Using Ion Mobility Spectrometry
May 6th 2025Ion mobility spectrometers can detect trace compounds quickly, though they can face various issues with detecting certain peaks. University of Hannover scientists created a new system for resolving hyper-fast gas chromatography (GC) peaks.
University of Oklahoma and UC Davis Researchers Probe Lipidomic Profiles with RP-LC–HRMS/MS
May 6th 2025A joint study between the University of Oklahoma Health Sciences Center (Oklahoma City, Oklahoma) and the UC Davis West Coast Metabolomics Center (Davis, California) identified differentially regulated lipids in type 2 diabetes (T2D) and obesity through the application of reversed-phase liquid chromatography-accurate mass tandem mass spectrometry (RP-LC-accurate MS/MS).
Automated Sample Preparation (ISO 20122) for MOSH/MOAH in Seasoning Oils
May 6th 2025This work presents an Automated Sample Preparation procedure for MOSH/MOAH analysis of Seasoning Oils. We compare results from a manual epoxidation procedure compliant with DIN 16995 with results based on fully automated sample preparation (epoxidation and saponification) compliant with ISO 20122. In both cases, online clean-up via activated aluminum oxide (AlOx) are used to remove interfering n-alkanes from the MOSH fraction during the HPLC run. Automated data evaluation using a dedicated software (GERSTEL ChroMOH) is presented.

.png&w=3840&q=75)

.png&w=3840&q=75)



.png&w=3840&q=75)



.png&w=3840&q=75)








