- The Column-06-20-2016
- Volume 12
- Issue 11
Smelling Arthritis
Gas chromatography–mass spectrometry (GC–MS) may be a viable diagnostic tool for inflammatory arthritis according to research from the University of Amsterdam.
Gas chromatography–mass spectrometry (GC–MS) may be a viable diagnostic tool for inflammatory arthritis according to research from the University of Amsterdam.1
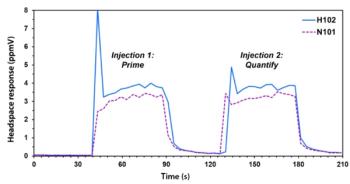
The study used an “electronic nose” (eNose) and GC–MS to detect volatile organic compounds (VOCs) specific to rheumatoid arthritis (RA) within the breathprints of patients. The VOCs act as markers of disease activity and allow the differentiation of RA from similar inflammatory joint diseases.
Affecting around 1% of the world population,2 RA has a wide-reaching impact and its prevalence increases with age - the average age of onset is 30–50 years old. The global trend of older populations has exacerbated the issue but little is conclusively known of the causes of RA. Genetic and lifestyle factors, such as smoking and obesity, have been proposed as important for disease development. The major issues surrounding RA are derived from diagnostic limitations; despite advances in novel diagnostic tools such as MRI and ultrasound,3,4 diagnosis of RA remains a convoluted process.
The earliest phases of RA are particularly challenging because of similarities with other inflammatory joint diseases and variable disease symptoms. Diagnosing RA early is essential to avoid therapeutic delay and the risk of irreversible damage to cartilage and bone. Furthermore, treatment regiments differ widely between RA and other inflammatory joint diseases so accurate diagnosis is crucial.
The method used in this new research focuses on unique VOCs, which are derived from multiple metabolic and inflammatory processes taking place within RA sufferers. As a systemic disease the likelihood of RA affecting the metabolites found in the lungs is high. Similar assertions have been demonstrated within asthma, chronic obstructive pulmonary disease (COPD),5 infectious diseases,6 and some forms of cancer.7,8,9
To utilize these metabolites researchers used an eNose, a device that allows highâthroughput analysis of gas mixtures, and GC–MS to visualize the full spectrum of VOCs. They hypothesized that such a device could differentiate between RA patients, psoriatic arthritis (PsA) patients, and healthy volunteers.
“In an ideal world we would imagine the eNose being a part of the care at the primary physician. So if a patient presents with arthritis, he or she could provide some exhaled breath and the eNose could assist in getting the right diagnosis, next to clinical signs and symptoms, and laboratory measurements such as BSE and antibody testing,” said Marjolein Brekelmans, Department of Vascular Medicine, University of Amsterdam, formerly of the Department of Clinical Immunology and Rheumatology, and lead author of the study.
Results indicated that the breathprints of RA patients could be distinguished from controls with an accuracy of 71%. Similar results were obtained when distinguishing PsA patients from controls (69%), and when distinguishing between RA and PsA patients (69%). In addition, GC–MS identified seven key VOCs that significantly differed between the groups.
Despite the positive nature of these results, by the authors’ own admission the eNose is far from ready for implementation into regular care for RA and PsA patients. “It is still in the research phase and external validation of the eNose in these patients must follow to confirm the results from our study,” continued Brekelmans.
Furthermore, the authors recommend a much larger examination of diagnostic accuracy in a large and untreated group of patients. This would address issues with baseline characteristics within the study.
Although a lot of work remains it is hoped that the non-invasive handheld device may eventually play a role in the diagnosis of RA, helping to provide fast diagnosis of an increasingly prevalent issue in modern populations.
Reference
- M.P. Brekelmans et al., PLoS One 11(3), e0151715 (2016).
- G. Firestein et al., Kelley’s textbook of rheumatology. (9th ed: Elsevier Saunders, 2013).
- P. Mandl et al., Rheumatology 53(12), 2136–2142 (2014).
- M.G. van de Sande et al., Rheumatology 51(7), 1240–1245 (2012).
- N. Fens et al., Clin. Exp. Allergy 43(7), 705–715 (2013).
- S. Sethi et al., Clin. Microbiol. Rev. 26(3), 462 –475 (2013).
- H. Haick et al., Chem. Soc. Rev. 43(5), 1423–1449 (2014).
- G. Peng et al., Br. J. Cancer 103(4), 542–551 (2010).
- M. Phillips et al., PLoS One 9(3), e90226 (2014).
Articles in this issue
over 9 years ago
Evaluating the Potential of HPLC with IMS-MS for Metabolomicsover 9 years ago
ChromSoc’s Lake District Lectures for Studentsover 9 years ago
Vol 12 No 11 The Column June 20, 2016 Europe and Asia PDFover 9 years ago
Vol 12 No 11 The Column June 20, 2016 North American PDFover 9 years ago
Leap Technologies and Antec Announce HDX–MS Ventureover 9 years ago
Celebrating the Career of Professor Klaus K. Ungerover 9 years ago
Are there any Holy Grails left in Chromatography?Newsletter
Join the global community of analytical scientists who trust LCGC for insights on the latest techniques, trends, and expert solutions in chromatography.